Background
Sickle cell disease (SCD) is at the intersection of social, racial, and healthcare equity in the US. It is a socially and medically complex disease associated with increased morbidity and mortality when compared to age, race, and sex matched persons without SCD. Despite a historically high prevalence, it has not been a priority in healthcare, which contributes to healthcare inequities in this population. Patients and clinicians consistently identify lack of clinician knowledge about SCD as a barrier to quality care. Providers describe discomfort managing patients and have a poor understanding of its complications. The number of physicians trained and available to treat adults with SCD is insufficient to meet population needs. With most hematology/oncology trained physicians choosing careers in oncology, the pool of practitioners with expertise in SCD is shrinking. This underscores the time-sensitive need for building an effective, sustainable, and patient-centered sickle cell educational curriculum early in training. At present, there is no widely used resource for SCD-specific education, and little research has been published describing physician education for this complex disease. This qualitative study is the first part of a two-part study which aims to serve as a needs assessment to understand the SCD specific educational demands of trainees and set the stage for survey development for wider distribution.
Methods
Residents applying for hematology/oncology fellowship and current fellows were recruited to participate in focus groups to explore trainees' preferences and attitudes for education on the management of patients with SCD. Trainees were recruited via email from seven academic institutions in the US from regions with a high prevalence of SCD. A focus group guide was developed inquiring about trainee perspectives on facilitators and barriers to obtaining sickle cell specific education. Using an inductive and iterative thematic analysis coding approach, all focus group transcripts were coded by an academic hematologist specializing in SCD (LV) and an academic psychiatrist specializing in SCD (EP). Codes were categorized and themes and subthemes developed.
Results
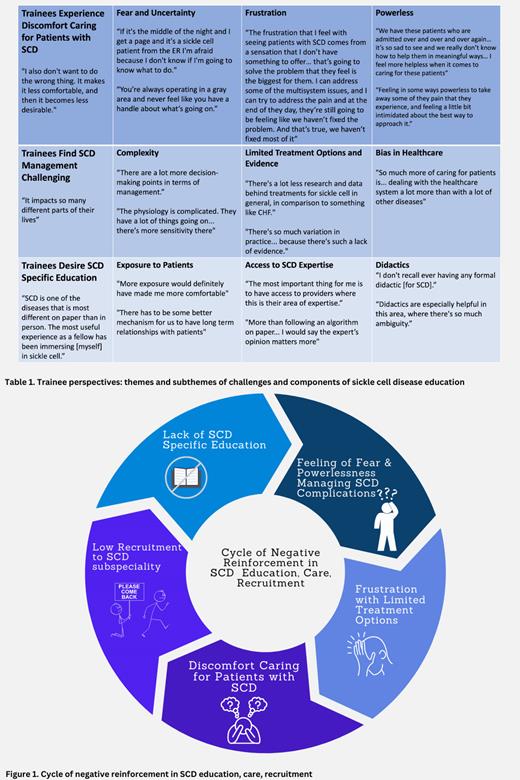
Four focus groups were conducted with a total of 15 participants (2 PGY 3 residents, and 13 hematology/oncology fellows PGY 4-6). Three themes were identified (Table): 1. Discomfort caring for patients with SCD. Trainees experienced feelings of fear, frustration, and powerlessness when caring for patients with SCD. 2. Challenges managing SCD. Trainees described the complexity of SCD management, limited treatment options and evidence-based practice, and navigating bias in healthcare as contributing to the challenge of treating patients with SCD. 3. Desire for SCD specific education during fellowship.Trainees noted ideal components of education should include exposure to patients longitudinally and in multiple settings, access to SCD expertise in the form of experts and expert guidelines, and SCD specific didactic content.
Conclusions
This study examined the experience of trainees with regards to SCD education and clinical care. Participants described how a lack of SCD specific education reinforced a cycle of discomfort and difficulty caring for patients with SCD (Figure). Lack of exposure to patients and access to experts impedes developing a sense of mastery in treating SCD. SCD education was underemphasized even at institutions with a high prevalence of SCD and a SCD program. Evidenced-based guidelines based on low evidence hinders self-directed learning. Overall, SCD specific education is under-emphasized in fellowship. Trainees who felt the most comfortable had a SCD specific curriculum integrated throughout the fellowship experience. A SCD specific curriculum in the form of case-based didactics and a SCD rotation, where feasible, should be built into hematology/oncology fellowship training to increase trainees' knowledge, comfort and therefore desire in caring for patients with SCD. This qualitative research study is the first of its kind and serves to set the stage for survey development to capture a larger needs assessment of the SCD specific educational demands of hematology/oncology fellows. Optimizing the care of persons with SCD requires a competent and confident workforce. This study provides key insights into the development of infrastructure to support such training.
Disclosures
Van Doren:Pharmacosmos Inc: Honoraria; Pfizer: Speakers Bureau; Daiichi Sankyo: Ended employment in the past 24 months; Sobi: Ended employment in the past 24 months; Sanofi: Ended employment in the past 24 months; GBT: Ended employment in the past 24 months.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal